Excessive Inflammation in MPN
WHAT DRIVES EXCESSIVE INFLAMMATION IN MPN?
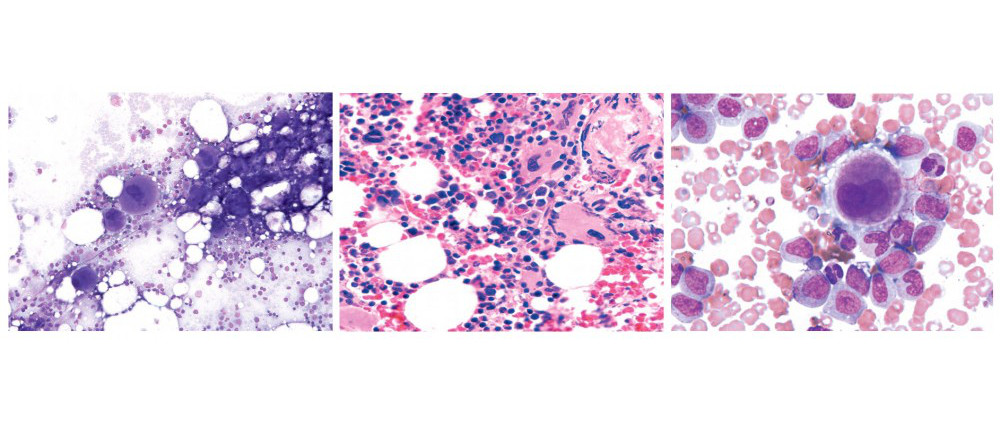
A deranged inflammatory cytokine profile is a central feature of myeloproliferative neoplasm. This excessive inflammatory state is responsible for the debilitating constitutional symptoms frequently observed in this disease. The JAK signaling pathway mediates this deranged inflammatory cytokine profile in MPN, as therapy with JAK inhibitors normalize inflammatory cytokines coincident with resolution of constitutional symptoms. Inflammation is not only responsible for the clinical consequences of MPN but is also critical for disease initiation.
We have identified a central role for the inflammatory cytokine tumor necrosis factor-alpha (TNF) in the clonal expansion of the JAK2V617F neoplastic clone in MPN. JAK2V617F endows upon hematopoietic stem cells TNF resistance, giving the JAK2V617F clone a selective advantage over their TNF sensitive JAK2WT counterparts. Targeting excessive TNF production is an attractive therapeutic target in MPN and would neutralize the selective advantage of the neoplastic clone leading to its contraction. Defining the mechanism by which TNF is overproduced in this disease is necessary to identify the most strategic way to target TNF overproduction.
TNF is classically produced by monocytes after stimulation through Toll-like receptor (TLR) engagement. TLRs are crucial pattern recognition receptors for microbial products that generate innate immune responses. There are a number of TLRs, each recognizing a conserved microbial structure. Upon TLR stimulation a signaling transduction cascade ensues, culminating in the production of inflammatory cytokines including TNF. The TLR pathway has tight negative regulation mechanisms to prevent the harmful effects of excessive inflammation. Stimulation through TLR activates a negative feedback cascade orchestrated by IL-10 and subsequent signaling via the JAK/STAT pathway. JAKs play an important role in the dampening of the TLR response, pharmacologic inhibition of JAKs lead to prolonged activation of the TLR signaling cascade and mice deficient in JAK fail to dampen TLR activation, leading to autoimmunity.
Because TLR signaling plays an integral role in inflammation and TNF production we hypothesized that an exaggerated signaling of the TLR signaling pathway is the mechanism by which TNF is overproduced in MPN. We quantified TLR responses in normal and MPN monocytes, reasoning that JAK2V617F might directly or indirectly influence the activation state of TLR modulatory factors. We found that monocytes from MPN patients have an exaggerated response to TLR agonists. We are currently working out exactly why MPN monocytes produce excessive TNF with the goal of developing therapies in MPN that will reduce this abnormal production of inflammatory cytokines.
Signalling cascades following TLR ligation
